Dr. Irfan Ali Motiwala* – MDS Oral and maxillofacial surgery, Dr. Motiwala Dental Clinic and Implant Center, Hyderabad, Telangana, India
Dr. Tejaswi Bathina – MDS, Oral Medicine and Radiology, Dr. Motiwala Dental Clinic and Implant Center, Hyderabad, Telangana, India
Available Online at: www.jcsmicasereports.org
Abstract
The use of single-piece basal implants in replacing missing teeth has many advantages over conventional multiunit dental implants. Good primary stability with minimal accumulation of plaque and/or bacteria around them is one among many others. Here, we present a case report of full mouth rehabilitation using single-piece basal implants in a patient with OSMF. Clinical limitations like reduced pliability of the mucosa and burning sensation limit fabricating a removable denture. Hence full mouth rehabilitation was done using implants in both jaws. The implants were immediately loaded with zirconia framework within three consecutive working days.
Keywords: Basal implants, OSMF, chronic periodontitis, laser fibrotomy, full mouth rehabilitation.
Background
The use of implant supported fixed prosthesis in partially or completely edentulous patients have gained popularity and many newer techniques have been made to overcome the disadvantages of the conventional Branemark system of implant placements. Basal implants or bicortical implants utilize the concept of engaging the highly dense basal bone, which offers greater primary stability and therefore favors immediate loading without any bone augmentation procedures2.
Oral submucous fibrosis is a chronic progressive potentially malignant disorder of the oral mucosa with the main etiological factor being areca nut chewing. The disease is characterized by a gradual reduction in mouth opening, stiffening of the oral mucosa, fibrous band formation along the buccal and labial mucosa, and burning sensation on taking food. Chronic periodontitis, on the other hand is most commonly seen in middle and older age groups, resulting in gradual loss of teeth, which further leads to compromised functional and esthetic components of an individual3, 4, 5.
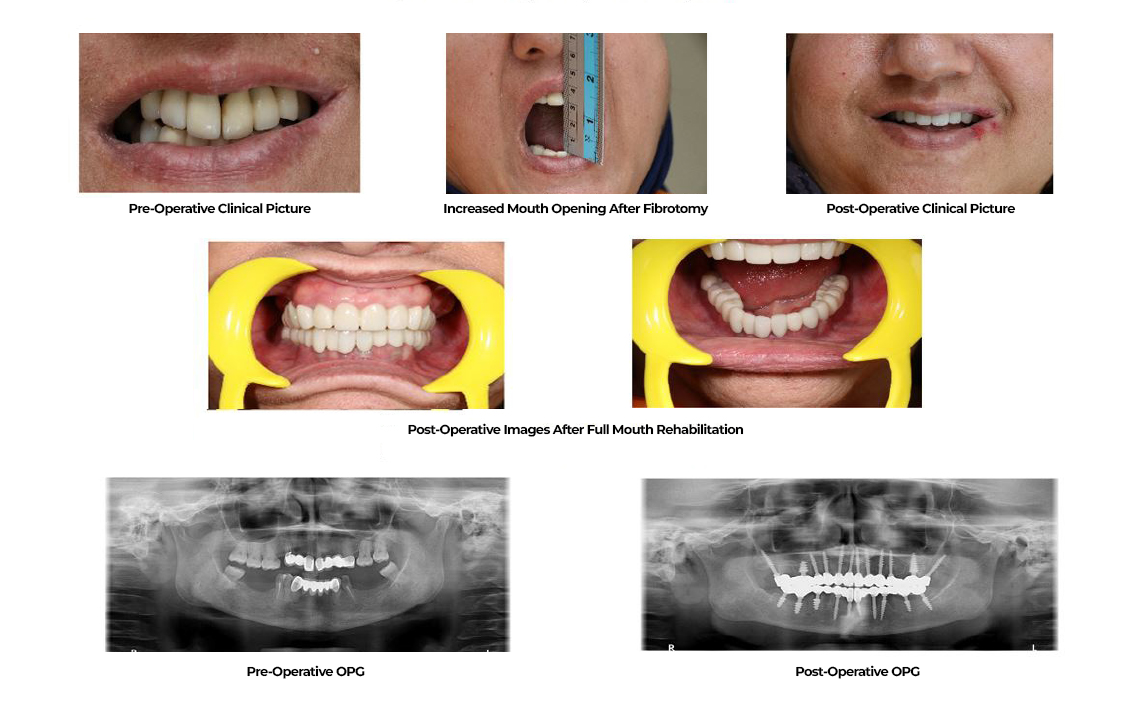
In this case report, the patient had a very poor periodontal condition with severely compromised functional ability and placement of any kind of dental instruments was challenging because of reduced mouth opening.[3] Hence the main objective of her treatment was to increase the mouth opening for which, bilateral fibrotomy was done along with intralesional corticosteroid injections therapy. Physiotherapy was strictly followed before and after the treatment to enhance the pliability of mucosa and mouth opening. Once the mouth opening was optimum, a total of twenty-two single-piece basal implants have been placed in the maxillary and mandibular arches with minimal intervention. The implants were immediately loaded with zirconia framework within three consecutive days.
Case Report
A 50-year-old female patient, partially edentulous, came to the clinic with a history of loss of teeth, loosening of remaining teeth and difficulty in chewing along with a burning sensation on taking hot and spicy food since 2 years. Her personal history revealed a habit of chewing supari for around 20 years and has stopped using it in the last 1 year. On thorough clinical examination, the patient was partially edentulous with missing teeth in relation to 15, 13, 12, 22, 23 and 25, supra-erupted teeth in relation to 16, 17, 11, 21, 26. The oral hygiene was poor with gingival inflammation and the periodontal status of remaining teeth was very poor. Generalized pallor and blanching was seen on the palate, buccal mucosa, and labial mucosa with vertical fibrous bands palpable on both sides. The mouth opening was reduced with an interincisal distance of 24mm.
Haematological investigations were made to rule out anemia or any other abnormalities. A provisional diagnosis of OSMF and chronic generalized periodontitis was given and the patient was thoroughly explained about the management of OSMF and various treatment options for the replacement of her teeth. The patient wanted to get a fixed prosthesis in a minimal amount of time. Since there was a generalized bone loss in both of the arches, and the prognosis was poor, extraction of the remaining teeth followed by full mouth rehabilitation with implants was suggested.
Management of OSMF
The patient had stage III OSMF with a reduced mouth opening of 24mm. this made it slightly difficult for placing any kind of dental instrument in her mouth. Hence the primary aim was to increase the mouth opening to an optimum level. To achieve that, the patient was initially counseled to strictly stop chewing any kind of tobacco products. Antioxidants (SM fibro- twice daily) and Intralesional injections consisting of 2ml dexamethasone, 1000IU hyaluronidase, and placentrex have been given twice weekly for two weeks. She was advised to do physiotherapy using wooden spatulas and blowing balloons (for at least an hour under a dentist’s supervision during the initial 2 weeks) 5-6 times a day until she experiences any discomfort. After this initial treatment, there was a slight improvement of 2 mm in the mouth opening.
Fibrotomy
Since the conventional treatment showed very little improvement in mouth opening, surgical intervention was planned after taking consent from the patient. Fibrotomy was performed with in pulse mode for initial demarcation of the bands followed by continuous mode to cut the bands[4]. Precise care was taken to include only the mucosal and submucosal areas without affecting the deeper layers. The procedure was performed starting from the pterygomandibular raphe and faucial pillars, continuing through the buccal mucosa at the level of occlusal plane. Primary closure of the surgical area was not done so as to allow the mucosa to epithelise on its own. An interincisal distance of 30mm was achieved immediately after the treatment and the patient was advised to continue physiotherapy. The mouth opening decreased to 25mm on the second postoperative day, as the patient did not do any jaw stretching exercise. Hence the patient was again counseled to strictly continue physiotherapy and topical corticosteroid (kenocart 0.1% cream thrice daily) was given. The mouth opening gradually increased to 28mm within the next 14 days and surgical intervention for implant placement was done on the following day.
Full Mouth Rehabilitation with Basal Implants:
A total of 16 teeth were present with fixed prostheses between 13 to 23 and 33 to 43. The remaining teeth were mobile with compromised periodontal status and hence were advised for extraction. Panoramic radiograph and CBCT scan were taken to identify suitable sites for implant placement. Extractions of the teeth have been done under local anesthesia followed by complete curettage of the sockets. Immediately after extraction, 12 maxillary (2pterygoid) and 10 mandibular single-piece basal implants were placed with minimal intervention using a flapless technique. Single-stage impressions of both arches were made using 3M ESPE monophase polyether impression material. Tentative intermaxillary records were made using high-viscosity polyvinylsiloxane (coltene jetbite) and temporization was done.
Casts were poured and the models have been mounted on the articulator. The casts were scanned using 3-shape CAD CAM and the zirconia framework was designed according to the intermaxillary relation. The following day, abutments were trimmed, accordingly and definitive intermaxillary records were taken. The overall length and bucco-lingual widths of the crowns were reduced to increase the space between the maxillary and the mandibular teeth and also to lessen the trauma, which will be implicated on the cheeks otherwise. The implants were functionally loaded with the final framework of glazed zirconia crowns using 3MESPE resin cement.
The patient was advised to continue physiotherapy and use antioxidants and multivitamins and is under follow-up. There has been a good improvement in the overall functional ability of the patient and no recurrence of trismus was noted.
Discussion
Using dental implants to replace missing teeth has become the most acceptable treatment modality because of its various advantages over the traditional removable and fixed tooth-supported prosthesis. However, the conventional system of crestal implant placement has many disadvantages among which the design of multiunit implants, with many interconnecting screws, delayed loading and the requirement of enough bone density and volume for the placement of an implant are the most common. This led to the improvement of the basic design of a dental implant to a single piece, which was initially developed by Dr.Gerard Scortecci in the year 1980 followed by several modifications5.
The conventional Branemark technique of implant placement utilizes the alveolar bone of the jaws that are more prone to resorb and/or lost as the teeth are removed or as the function reduces. Basal implants on the other hand are inserted into the basal bone. Unlike the alveolar bone, it is less likely to resorb, gives an excellent support for the implants and the low vascularity makes it less prone to infections6.
As the implants are engaged into the highly corticated basal bone, primary stability is easily achieved and hence immediate loading of the implants can be done with a high success rate. In this case, the patient had stage III OSMF with a burning sensation and fibrous bands palpable on both sides of the buccal mucosa5,6.
Removable prosthetic complete dentures may also serve the purpose of mainting the functional ability of the patient. However, chronic mucosal irritation in patients with osmf that can be caused by sharp teeth, dentures and/or the conventional implants with its multiunit design, increases the risk of malignant transformation, which is around 3% to 16%. [7,8]
Rehabilitation using dental implants can be challenging when there is reduced mouth opening. Patients with certain potentially malignant disorders like OSMF, tend to neglect their oral hygiene due to discomfort caused during performing general oral hygiene measures like brushing. This leads to an increased occurrence of gum diseases, which gradually reduces their functional ability [9].
Replacing teeth with conventional multiunit implants in such patients might worsen the condition as they may cause physical trauma to the surrounding mucosal structures. These patients also have difficulty in maintaining good oral hygiene with an accumulation of plaque and bacteria between the minute gaps. Hence single piece implants were chosen for this patient as they have a long neck and a smooth surface, which is less prone to bacterial attack and reduce bacterial colonization in patients who are prone to gum diseases10. Twelve implants engaging the basal bone were placed in the maxillary jaw using the flapless technique out of which two were placed in the pterygoid region to avoid the sinus margin and ten basal implants were placed in the mandibular arch.
The framework of teeth was fabricated using monolith anatomical zirconium. The overall size of the fabricated teeth was also reduced with only a little change in the vertical dimension to enhance the functional ability of the patient. The use of monolith zirconia has the advantage of being the most biocompatible material with good mechanical properties11. Their good mechanical properties make them less prone to chip off when chewing hard food. They are highly esthetic mimicking the natural teeth.
Pre & Post Operative Pictures of the Patient
Conclusion
The concept of single-piece basal implants remains the very first option with many advantages, whenever there is a need for augmentation procedures. Single-piece implants with long polished necks remain to be the best mode of replacing teeth in patients with potentially malignant conditions like some who generally have difficulty in maintaining oral hygiene status and are prone to gum diseases.
References
1) Ghalaut P, Shekhawat H, Meena B. Full-mouth rehabilitation with immediate loading basal implants: A case report. Natl J Maxillofac Surg. 2019;10(1):91–94.
2) Aakarshan Dayal Gupta, Aviral Verma, Tanay Dubey, Saloni Thakur. Basal osseointegrated implants: classification and review. International Journal of Contemporary Medical Research 2017;4(11):2329-2335
3) Kajave M, Shingote S, Mankude R, Chodankar K. An innovative prosthodontic approach in managing oral submucous fibrosis patient. SRM J Res Dent Sci 2015;6:139-43
4) Sana Farista1 , Butchibabu Kalakonda, SHANIN FARISTA , Vidyaa Hari Iyer. Diode Laser-Assisted Fibrotomy in the Management of Oral Sub-Mucous Fibrosis: A New Technique in Surgical Management Journal of Clinical and Diagnostic Research. 2018 Jul, Vol-12(7): ZH01-ZH02
5) Kumar K, Kumar S, Singh R, Vaibhav V, Kedia NB, Singh AK. Basal implants- A new era of prosthodontic dentistry. IP Ann Prosthodont Restor Dent. 2020;6(1):1-3.
6) Motiwala, Irfan Ali; Bathina, Tejaswi1. A Radiographic Study on Pterygoid Implants with Hamulus as a Landmark for Engaging the Pterygoid Plate – A Retrospective Study. Annals of Maxillofacial Surgery 12(2):p 190-196, Jul–Dec 2022. | DOI: 10.4103/ams.ams_132_22
7) Jena AK, Rautray S, Mohapatra M, Singh S. Oral health-related quality of life among male subjects with oral submucous fibrosis in a tertiary care hospital. Indian J Public Health 2018;62:271-6
8) Hegde S, Anuradha A, Asha V: Malignant transformation of oral submucous fibrosis. J Med Radiol Pathol Surg. 2015, 1:32-36. 1
9) Burde NN, Kour P. Oral submucous fibrosis – an impediment for maintenance of good oral hygiene: A questionnaire-based study. J Adv Clin Res Insights 2019;6: 106-109
10) Dr. Irfan Ali Motiwala, Dr. TejaswiBathina, “Prognosis of a Polished Ssurface Basal Implant”, IJDSIR- June – 2022, Vol. – 5, Issue – 3, P. No. 515 – 520.
11) Tang Z, Zhao X, Wang H, Liu B. Clinical evaluation of monolithic zirconia crowns forposterior teeth restorations. Medicine. 2019;98:40(e17385)